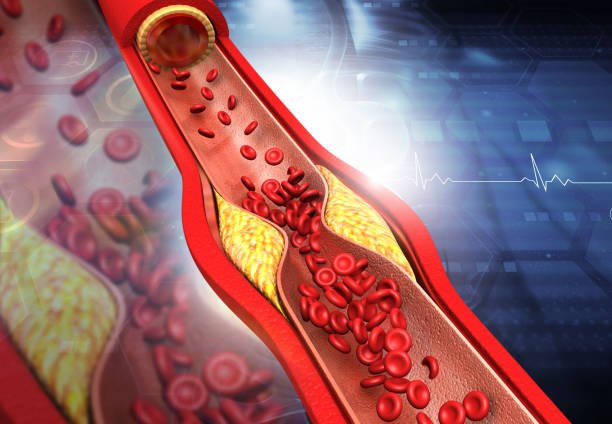
Atherosclerosis is a medical condition characterized by the gradual buildup of plaque deposits within the walls of arteries. These plaques contain cholesterol, fatty substances, cellular waste, calcium, and other substances. Over time, the accumulation of these deposits can lead to the narrowing and hardening of the arteries, restricting blood flow to organs and tissues.
Pathological changes:
The process of atherosclerosis begins when there is damage or inflammation in the inner lining of the arteries. In response to this damage, substances like cholesterol and inflammatory cells migrate to the site, forming a plaque. As the plaque grows, it can impede blood flow and, in some cases, lead to the formation of blood clots. If a blood clot completely blocks an artery, it can result in a heart attack or stroke, depending on the location of the affected artery.
Causes of atherosclerosis:
Atherosclerosis is a common underlying factor in various cardiovascular diseases, including coronary artery disease, peripheral artery disease, and cerebrovascular disease. Risk factors for developing atherosclerosis include high blood pressure, high cholesterol levels, smoking, diabetes, and a family history of cardiovascular diseases. Lifestyle modifications, medication, and medical interventions may be employed to manage atherosclerosis and reduce the risk of related complications.
Symptoms:
Angina: Chest pain or distress that happens when the heart muscle doesn’t get sufficient blood. It might feel like tension, pressing, or totality in the chest. In many cases, actual effort or close home pressure can cause angina.
Shortness of Breath: Reduced blood flow to the heart muscle can lead to difficulty breathing, especially during physical activity.
Heart Attack (Myocardial Infarction): If a blood clot completely blocks an artery that supplies blood to the heart, it can cause a heart attack. Symptoms include chest pain, shortness of breath, sweating, nausea, and lightheadedness.
Stroke: Atherosclerosis in the arteries that supply the brain can lead to a stroke. Symptoms may include sudden weakness or numbness on one side of the body, difficulty speaking, confusion, and vision problems.
Peripheral Artery Disease (PAD): Atherosclerosis in the arteries supplying the limbs, particularly the legs, can cause pain, numbness, and weakness in the affected limbs. This is termed as peripheral artery disease.
Chronic Kidney Disease (CKD): Atherosclerosis affecting the renal arteries can lead to kidney damage over time. Symptoms may include changes in urine output, fluid retention, and high blood pressure.
Erectile Dysfunction (ED): Atherosclerosis can also affect the blood vessels supplying the reproductive organs, leading to erectile dysfunction in men.
Atherosclerosis in different age groups:
Childhood and Adolescence: Atherosclerosis can begin in childhood, and the early stages may involve the deposition of fatty streaks in the arterial walls.
Factors such as genetics, diet, and lifestyle habits can influence the development of atherosclerosis in young individuals.
Childhood obesity, lack of physical activity, and poor dietary choices can contribute to the early onset of risk factors like elevated cholesterol levels.
Young Adults (20s to 40s): Atherosclerosis may progress slowly during these years, and symptoms are usually absent.
Risk factors such as smoking, high blood pressure, diabetes, and high cholesterol levels can accelerate the development of atherosclerosis in this age group.
Lifestyle choices and preventive measures become crucial to manage risk factors and slow down the progression of the disease.
Middle Age (40s to 60s): Atherosclerosis tends to become more apparent during middle age, with symptoms possibly manifesting.
Plaque buildup can lead to reduced blood flow, causing symptoms like chest pain (angina) or shortness of breath.
Regular medical check-ups and screenings become important to monitor and manage cardiovascular risk factors.
Older peoples (60s and beyond): Atherosclerosis is more prevalent in older adults, and its complications can become more serious.
Increased risk of heart attacks, strokes, and other cardiovascular events may occur.
Advanced stages may lead to the need for interventions like angioplasty, stent placement, or coronary artery bypass grafting (CABG).
Diagnostic Techniques for Atherosclerosis:
Medical History and Physical Examination:
A thorough review of the patient’s medical history, risk factors, and symptoms.
Physical examination to check for signs of cardiovascular disease, such as high blood pressure, abnormal heart sounds, or evidence of arterial disease.
Blood Tests:
Lipid profile tests measure cholesterol levels, including low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
High-sensitivity C-reactive protein (hs-CRP) test to assess inflammation, which is associated with atherosclerosis.
Electrocardiogram (ECG or EKG):
Records the electrical activity of the heart, helping to identify irregularities or signs of ischemia (lack of blood flow to the heart muscle).
Echocardiography:
Uses sound waves to create images of the heart, providing information about its structure and function, including blood flow and potential abnormalities.
Stress Testing:
Measures the heart’s response to physical stress to detect signs of reduced blood flow that may be indicative of coronary artery disease.
CT Angiography (CTA):
Involves the use of computed tomography to create detailed images of the coronary arteries, helping to identify plaque buildup and arterial narrowing.
MRI (Magnetic Resonance Imaging):
Can provide detailed images of the heart and blood vessels, helping to evaluate blood flow and detect abnormalities.
Carotid Ultrasound:
Uses sound waves to create images of the carotid arteries in the neck, assessing blood flow and detecting plaques that may increase the risk of stroke.
Peripheral Arterial Disease (PAD) Tests:
Ankle-brachial index (ABI) measurement compares blood pressure in the ankle and arm to assess peripheral artery disease.
Invasive Angiography:
Involves injecting a contrast dye into the blood vessels to visualize the coronary arteries, providing detailed images and helping to identify blockages.
Treatments for atherosclerosis:
The treatment of atherosclerosis aims to manage the condition, reduce symptoms, prevent complications, and lower the risk of cardiovascular events. Treatment approaches may involve lifestyle modifications, medications, and, in some cases, surgical interventions. Here are common strategies used in the management of atherosclerosis:
Lifestyle Modifications:
Dietary Changes: Adopting a heart-healthy diet that is low in saturated and trans fats, cholesterol, and sodium. Consume fruits, vegetables, entire grains, and lean proteins.
Regular Exercise: Engaging in regular physical activity to promote cardiovascular health and manage weight. Aim for at least 150 minutes of moderate-power practice each week.
Smoking Cessation: Quitting smoking is crucial, as smoking contributes to the progression of atherosclerosis and increases the risk of cardiovascular events.
Medications:
Statins: These drugs lower cholesterol levels and are commonly prescribed to reduce the risk of cardiovascular events.
Antiplatelet Medications: Aspirin or other antiplatelet drugs may be recommended to reduce the risk of blood clots.
Antihypertensive Medications: Controlling high blood pressure is essential to prevent further damage to arteries.
Anticoagulants: In some cases, anticoagulant medications may be prescribed to prevent blood clots.
Management of Diabetes:
For individuals with diabetes, maintaining good blood sugar control is essential to reduce the impact of diabetes on blood vessels.
Weight Management:
Accomplishing and keeping a sound weight is significant for generally speaking cardiovascular wellbeing.
Surgical Interventions:
Angioplasty and Stenting: In cases of significant arterial blockages, a procedure called angioplasty may be performed to open the narrowed artery, often accompanied by the placement of a stent to keep the artery open.
Coronary Artery Bypass Grafting (CABG): For more extensive disease, CABG may be recommended. This involves bypassing blocked arteries using blood vessels from other parts of the body.
Management of Complications:
Treating complications such as peripheral artery disease, carotid artery disease, or aneurysms may require specific interventions tailored to the affected arteries.

Pingback: Ischemic cardiomyopathy treatment - Pharmacyinfos