Understanding about ischemic cardiomyopathy:
Ischemic cardiomyopathy refers to a condition where the heart muscle (myocardium) becomes weakened and dysfunctional due to inadequate blood supply, typically resulting from coronary artery disease (CAD) or other conditions that obstruct or reduce blood flow to the heart muscle.
In ischemic cardiomyopathy, the heart muscle is deprived of oxygen and nutrients, leading to damage and impaired function. Over time, this can lead to heart failure, where the heart is unable to pump blood effectively to meet the body’s needs.

The main causes and risk factors associated with ischemic cardiomyopathy include:
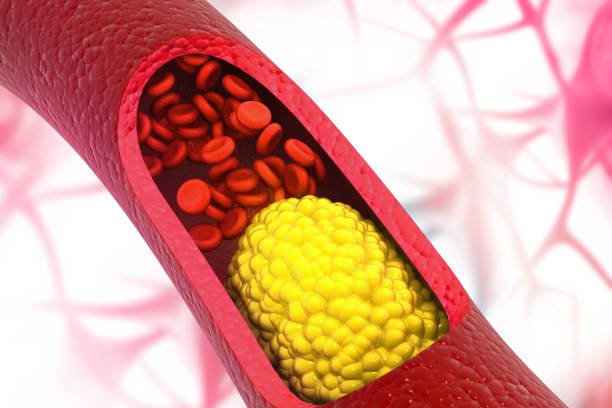
Coronary Artery Disease (CAD): CAD is the most common cause of ischemic cardiomyopathy. Atherosclerosis, which involves the accumulation of plaque made up of cholesterol, fat, and other substances in the coronary arteries, can restrict blood flow to the heart.
Heart Attack (Myocardial Infarction): A heart attack occurs when a coronary artery becomes suddenly blocked, cutting off blood supply to a part of the heart muscle. If not promptly treated, a heart attack can lead to permanent damage to the heart muscle, contributing to ischemic cardiomyopathy.
Chronic Hypertension (High Blood Pressure): High blood pressure can strain the heart and lead to thickening and stiffening of the heart muscle over time, impairing its ability to pump blood effectively.
Diabetes Mellitus: Diabetes is a risk factor for atherosclerosis and can lead to damage to the blood vessels, including the coronary arteries, increasing the risk of ischemic cardiomyopathy.
Smoking: Smoking is a major risk factor for CAD and can accelerate the progression of atherosclerosis, further compromising blood flow to the heart.
High Cholesterol Levels: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL) cholesterol, can contribute to the development of atherosclerosis and increase the risk of ischemic cardiomyopathy.
Obesity: Obesity is associated with several risk factors for ischemic cardiomyopathy, including hypertension, diabetes, and dyslipidemia (abnormal levels of lipids in the blood), which can all contribute to the development of CAD.
Sedentary Lifestyle: Lack of regular physical activity can contribute to obesity, hypertension, and other risk factors for ischemic cardiomyopathy.
Family History: A family history of heart disease, particularly premature coronary artery disease, can increase the risk of developing ischemic cardiomyopathy.
Age and Gender: Advancing age and being male are additional risk factors for developing ischemic cardiomyopathy, although it can affect individuals of any age and gender.
Symptoms:
Chest Pain or Discomfort: This is typically the hallmark symptom of coronary artery disease. The chest pain, known as angina, may feel like pressure, tightness, squeezing, or burning in the chest. It may also radiate to the arms, shoulders, neck, jaw, or back.
Shortness of Breath: Difficulty breathing, especially during physical activity or exertion, is a common symptom of ischemic cardiomyopathy. This symptom may cause serious effects over time as the condition progresses.
Fatigue: Feeling unusually tired or fatigued, even after rest, is another common symptom of ischemic cardiomyopathy. This fatigue may be persistent and interfere with daily activities.
Swelling (Edema): Fluid retention, leading to edema or swelling in the legs, ankles, feet, or abdomen, can occur as the heart becomes less efficient at pumping blood. This swelling may worsen throughout the day or be more noticeable after periods of inactivity.
Irregular Heartbeat (Arrhythmias): Ischemic cardiomyopathy can disrupt the heart’s normal electrical impulses, leading to irregular heart rhythms such as atrial fibrillation, ventricular tachycardia, or ventricular fibrillation. These arrhythmias may cause palpitations, dizziness, lightheadedness, or fainting.
Dizziness or Lightheadedness: Reduced blood flow to the brain due to poor heart function can cause dizziness or lightheadedness, especially when standing up quickly or exerting oneself.
Reduced Exercise Tolerance: People with ischemic cardiomyopathy may experience a decreased ability to tolerate physical activity due to reduced heart function and poor circulation.
Treatment options for ischemic cardiomyopathy:
Medications:
Angiotensin-converting enzyme (ACE) inhibitors: Examples include medications such as lisinopril, enalapril, ramipril, and captopril. ACE inhibitors block the action of angiotensin-converting enzyme, which normally converts angiotensin I into angiotensin II. Angiotensin II is a potent vasoconstrictor that causes blood vessels to narrow, leading to high blood pressure.
By inhibiting the formation of angiotensin II, ACE inhibitors cause blood vessels to dilate, reducing blood pressure and decreasing the workload on the heart.
Beta-blockers: Beta-blockers are a class of medications commonly used in the treatment of various cardiovascular conditions, including ischemic cardiomyopathy.
These drugs work by blocking the effects of adrenaline (epinephrine) and other stress hormones on the heart, thereby reducing heart rate and blood pressure, and improving heart function.
For example: Metoprolol, Carvedilol, Bisoprolol, Atenolol, Propranolol.
Diuretics: Diuretics are commonly used in the management of ischemic cardiomyopathy to alleviate symptoms of fluid overload and congestion, which are characteristic features of heart failure.
Diuretics help reduce this fluid overload by increasing urine output, thereby decreasing the volume of fluid in the body.
furosemide (Lasix), bumetanide (Bumex), and torsemide (Demadex) are commonly prescribed to decrease fluid retention in patients with ischemic cardiomyopathy.
Aldosterone antagonists: Aldosterone antagonists, also known as mineralocorticoid receptor antagonists (MRAs), are a class of medications commonly used in the management of heart failure, including ischemic cardiomyopathy. These medications work by blocking the effects of aldosterone, a hormone that plays a key role in regulating sodium and water balance in the body.
For example: spiranolactone and eplerenone is one of the aldosterone antagonist help reduce fluid retention and edema, thereby alleviating symptoms of congestion and improving overall heart failure symptoms.
Anticoagulants: Anticoagulants are medications that help prevent the formation of blood clots or reduce the risk of existing blood clots from growing larger. In the context of ischemic cardiomyopathy, anticoagulants may be used for several reasons, primarily to reduce the risk of thromboembolic events such as strokes and systemic embolisms.
Example of anticoagulants: Warfarin, Dabigatran,Rivaroxaban,Apixaban,Edoxaban,
Statin drugs: Statins used to lower cholesterol levels and reduce the risk of further plaque buildup in the arteries. Statins help lower low-density lipoprotein (LDL) cholesterol, also known as “bad” cholesterol, which is a major contributor to the development of atherosclerosis.
By reducing LDL cholesterol levels, statins can slow the progression of atherosclerosis, stabilize existing plaque, and decrease the risk of further coronary artery narrowing or blockages.
Example of statin drug:
Atorvastatin
Simvastatin
Rosuvastatin
Pravastatin
Lovastatin
Surgical treatment for ischemic cardiomyopathy:
Surgical treatment for ischemic cardiomyopathy aims to improve blood flow to the heart muscle or correct structural abnormalities that may contribute to heart failure.
Here are some common surgical treatments:
Coronary Artery Bypass Grafting (CABG): CABG surgery involves bypassing blocked or narrowed coronary arteries using blood vessels harvested from elsewhere in the body. By creating new pathways for blood flow to the heart muscle, CABG can relieve ischemia and improve heart function.
Percutaneous Coronary Intervention (PCI): Also known as coronary angioplasty or stenting, PCI involves inserting a catheter with a balloon at the tip into the blocked coronary artery. The balloon is then inflated to compress the plaque against the artery walls, broadening the artery and restoring blood flow. Sometimes, a stent (a mesh tube) is placed to keep the artery open.
Ventricular Restoration Surgery: In some cases of advanced ischemic cardiomyopathy where the heart has become enlarged and distorted, ventricular restoration surgery may be performed. This surgery aims to reshape and reduce the size of the enlarged ventricle, improving its efficiency.
Heart Transplantation: For severe cases of ischemic cardiomyopathy where other treatments have failed, heart transplantation may be considered. This includes replacing the diseased heart with a healthy donor heart.
Left Ventricular Assist Device (LVAD): In cases where heart transplantation is not immediately feasible, an LVAD may be implanted to assist the heart in pumping blood. This device helps improve heart function and can serve as a bridge to transplant or as destination therapy for those who are not candidates for transplantation.
Enhanced External Counterpulsation (EECP): While not a surgical procedure, EECP is a non-invasive treatment option for ischemic cardiomyopathy. It involves the use of inflatable cuffs wrapped around the patient’s legs that inflate and deflate in sync with the heartbeat, enhancing blood flow to the heart muscle.
