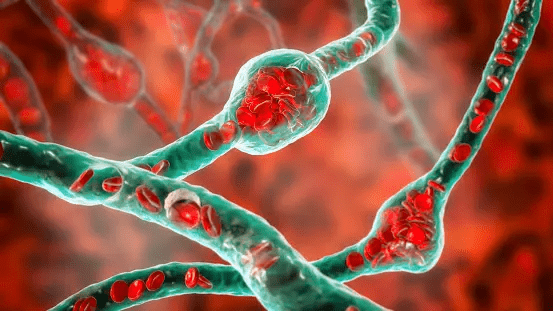
A brain aneurysm, also known as a cerebral aneurysm or intracranial aneurysm, is a bulging or ballooning in a blood vessel in the brain. These weak spots in the blood vessel wall can develop over time due to various factors, including genetic predisposition, high blood pressure, smoking, and certain medical conditions.
Brain aneurysms can vary in size and shape. Some are small and may not cause any symptoms or issues, while others can be larger and pose a risk of rupture, leading to potentially life-threatening bleeding into the brain (hemorrhagic stroke) or surrounding areas.
The symptoms of an unruptured brain aneurysm may not be noticeable, but when an aneurysm ruptures, it can cause a sudden, severe headache, nausea, vomiting, sensitivity to light, loss of consciousness, and other neurological symptoms.
Symptoms of brain aneurysm:
Brain aneurysms can often go unnoticed, particularly if they are small and not causing any symptoms. However, when symptoms do occur, they can vary depending on whether the aneurysm has ruptured or not. Here are the common symptoms associated with both unruptured and ruptured brain aneurysms:
Unruptured Brain Aneurysm:
Asymptomatic: Many brain aneurysms are discovered incidentally during imaging tests conducted for unrelated reasons, and they may not cause any symptoms at all.
Localized Symptoms: In some cases, an unruptured brain aneurysm may cause localized symptoms due to its size or location, such as:
- Headaches
- Eye pain or vision changes
- Facial pain or numbness
- Dilated pupils
- Difficulty speaking
- One side of face or body experiencing weakness or paralysis
- Cognitive impairment or memory problems
Ruptured Brain Aneurysm (Subarachnoid Hemorrhage):
Sudden, Severe Headache: Often described as the worst headache of one’s life, this headache may come on suddenly and intensely.
Nausea and Vomiting: Individuals may experience nausea and vomiting, sometimes accompanied by a feeling of sickness.
Stiff Neck: A stiff neck or neck pain may occur due to irritation of the meninges (the membranes covering the brain and spinal cord) by blood from the ruptured aneurysm.
Sensitivity to Light (Photophobia): Bright lights may exacerbate symptoms, leading to discomfort or pain in the eyes.
Altered Mental State: Confusion, disorientation, or loss of consciousness may occur, particularly in severe cases.
Seizures: Some individuals may experience seizures, which can manifest as involuntary muscle movements, loss of consciousness, or unusual sensations.
Focal Neurological Deficits: Depending on the location of the aneurysm and the extent of bleeding, individuals may experience focal neurological deficits such as weakness, numbness, or paralysis on one side of the body, difficulty speaking or understanding language, or visual disturbances.
Causes and risk factors of brain aneurysm:
Weakness in Blood Vessel Walls: Aneurysms occur when there is a weakening or thinning of the walls of blood vessels in the brain. This weakness can be congenital (present at birth) or acquired over time due to factors such as aging, high blood pressure, or atherosclerosis (hardening of the arteries).
Genetic Factors: There is evidence to suggest that genetic factors play a role in the development of brain aneurysms. People with a family history of aneurysms or certain genetic disorders such as polycystic kidney disease, Ehlers-Danlos syndrome, or Marfan syndrome may have an increased risk.
Gender and Age: Brain aneurysms are more common in women than in men, and the risk tends to increase with age. However, aneurysms can occur at any age, including in children.
High Blood Pressure (Hypertension): Chronic high blood pressure can weaken blood vessel walls over time, increasing the risk of developing an aneurysm.
Smoking: Tobacco use, including smoking cigarettes or using other forms of tobacco, is a significant risk factor for the development and rupture of brain aneurysms. Smoking can damage blood vessels and increase the risk of aneurysm formation and rupture.
Heavy Alcohol Consumption: Excessive alcohol consumption has been linked to an increased risk of developing brain aneurysms, as it can raise blood pressure and weaken blood vessel walls.
Drug Abuse: The use of certain drugs, particularly cocaine and amphetamines, has been associated with an increased risk of brain aneurysms due to their effects on blood vessels and blood pressure.
Trauma: Head injuries or trauma to the brain can sometimes lead to the formation or rupture of aneurysms, particularly in cases of severe or repeated trauma.
Certain Medical Conditions: Conditions such as arteriovenous malformations (AVMs), infections, tumors, and other vascular diseases can increase the risk of developing brain aneurysms.
Pregnancy and Hormonal Changes: Hormonal changes during pregnancy and the use of hormonal contraceptives or hormone replacement therapy may contribute to the development or rupture of brain aneurysms, although the exact mechanisms are not fully understood.
Diagnostic methods for brain aneurysm:
Diagnostic methods for brain aneurysms are crucial for identifying these potentially life-threatening conditions.
Here are the primary diagnostic methods used:
Imaging Techniques:
- CT Scan (Computed Tomography): A CT scan can detect the presence of a brain aneurysm, especially if it has ruptured and caused bleeding in the brain. It provides detailed images of the brain’s structures and can help identify the location and size of the aneurysm.
- Magnetic Resonance Imaging (MRI): MRI uses powerful magnets and radio waves to produce detailed images of the brain. It can provide clearer images of blood vessels and is useful for detecting both unruptured and ruptured aneurysms.
- Magnetic Resonance Angiography (MRA): MRA is a specialized MRI technique that focuses on imaging blood vessels. It can provide detailed images of the blood vessels in the brain, including any abnormalities such as aneurysms.
Cerebral Angiography (Digital Subtraction Angiography – DSA): This is an invasive procedure where a contrast dye is injected into the blood vessels, followed by X-rays to visualize the blood flow in the brain. It provides highly detailed images of blood vessels and is considered the gold standard for diagnosing brain aneurysms.
Lumbar Puncture (Spinal Tap): In some cases, a lumbar puncture may be performed to analyze the cerebrospinal fluid for signs of bleeding, which can indicate a ruptured aneurysm.
Clinical Assessment and Neurological Examination: A thorough medical history, physical examination, and neurological assessment are essential for evaluating symptoms and signs that may indicate the presence of a brain aneurysm, such as sudden severe headache, visual problems, nausea, vomiting, and neurological deficiencies.
Screening Tests: In certain high-risk populations or individuals with a family history of brain aneurysms, screening tests such as CT angiography (CTA) or magnetic resonance angiography (MRA) may be performed to detect asymptomatic aneurysms before they rupture.
Genetic Testing: In cases where there is a suspected genetic predisposition to brain aneurysms (e.g., certain hereditary conditions such as autosomal dominant polycystic kidney disease), genetic testing may be considered to identify specific genetic mutations associated with an increased risk of aneurysm formation.
Brain aneurysm treatment without surgery:
Endovascular Coiling:
Endovascular coiling is a minimally invasive procedure used to treat brain aneurysms. It involves inserting a catheter into an artery, usually in the groin, and guiding it through the blood vessels to the site of the aneurysm in the brain. Endovascular coiling is a widely used and effective treatment option for many types of brain aneurysms, offering advantages such as shorter recovery times, reduced risk of complications compared to open surgery, and excellent long-term outcomes for appropriately selected patients. However, it may not be suitable for all aneurysm types and locations, and treatment decisions should be individualized based on factors such as aneurysm morphology, patient age, overall health, and preferences.
Intra-Aneurysmal Embolization:
Intra-aneurysmal embolization, also known as endovascular embolization or simply embolization, is a minimally invasive procedure used to treat brain aneurysms. It involves the injection of embolic agents into the aneurysm sac to induce clot formation and thereby block blood flow into the aneurysm, preventing the risk of rupture.
Here’s how the procedure generally works:
Preparation: Before the procedure, the patient undergoes imaging studies such as cerebral angiography or CT angiography to precisely locate the aneurysm and assess its size, shape, and surrounding blood vessels. The patient is also prepared for the procedure with fasting and medication management as needed.
Anesthesia: Intra-aneurysmal embolization is typically performed under local anesthesia, although general anesthesia may be used in some cases depending on the patient’s condition and preferences.
Catheter Insertion: A small incision is made in the groin area, and a catheter (a long, thin tube) is inserted into a large artery, usually the femoral artery, under fluoroscopic guidance. The catheter is then carefully advanced through the arterial system and into the blood vessels of the brain.
Navigation to the Aneurysm: Using real-time X-ray guidance (fluoroscopy) and contrast dye injections, the neurointerventional surgeon navigates the catheter through the arteries until it reaches the location of the aneurysm in the brain.
Embolization: Once the catheter is positioned at the aneurysm site, embolic agents are injected through the catheter and into the aneurysm sac. These embolic agents can take various forms, including detachable coils, liquid embolic agents (such as Onyx or n-Butyl cyanoacrylate glue), or synthetic materials (such as polyvinyl alcohol particles). The choice of embolic agent depends on factors such as the size and shape of the aneurysm and the surgeon’s preference.
Assessment: After embolization, a final angiogram (cerebral angiography) is performed to confirm the placement of the embolic agents and assess blood flow within the treated aneurysm and surrounding vessels. This helps ensure that the aneurysm has been effectively occluded and there are no complications such as unintended blockage of normal blood vessels or residual filling of the aneurysm.
Closure: Once the procedure is completed, the catheter is removed, and pressure is applied to the incision site to prevent bleeding. In some cases, a closure device may be used to seal the artery puncture site.
Recovery: Following the procedure, patients are typically monitored in a recovery area for a few hours to ensure stability before being discharged home. Most patients can resume normal activities within a few days, although strenuous physical exertion should be avoided for a period of time as advised by the healthcare provider.
Radiosurgery for Brain Aneurysms:
Radiosurgery for brain aneurysms is a non-invasive treatment approach that uses highly focused beams of radiation to target and treat the aneurysm. Unlike conventional surgical techniques, radiosurgery does not involve incisions or the insertion of catheters into the body. Instead, it delivers precise doses of radiation to the aneurysm, causing it to gradually close off over time.
Here’s an overview of how radiosurgery for brain aneurysms typically works:
Patient Evaluation: Before undergoing radiosurgery, patients undergo a thorough evaluation by a multidisciplinary team of specialists, including neurosurgeons, radiation oncologists, and neuroradiologists. This evaluation includes a review of the patient’s medical history, imaging studies (such as MRI or CT angiography) to assess the size, location, and morphology of the aneurysm, and other relevant factors such as the patient’s overall health and risk factors.
Treatment Planning: Based on the patient’s evaluation, a treatment plan is developed to deliver precisely targeted radiation to the aneurysm while minimizing exposure to surrounding healthy brain tissue. Advanced imaging techniques and computer software are used to map out the treatment area and calculate the optimal radiation dose.
Radiosurgery Delivery: During the radiosurgery procedure, the patient is positioned on a treatment table, and a specialized machine, such as a Gamma Knife or CyberKnife system, is used to deliver highly focused beams of radiation to the aneurysm. The radiation is delivered from multiple angles to ensure precise targeting of the aneurysm while sparing nearby structures.
Follow-up Monitoring: After undergoing radiosurgery, patients are typically monitored closely with periodic imaging studies (such as MRI or CT angiography) to assess the response of the aneurysm to treatment and detect any potential complications. It may take several months or longer for the aneurysm to fully close off, and follow-up imaging helps track the progress of treatment.
Outcome Assessment: The effectiveness of radiosurgery for brain aneurysms is typically assessed based on the closure rate of the aneurysm, as determined by follow-up imaging studies, as well as clinical outcomes such as the prevention of aneurysm rupture and resolution of symptoms. In some cases, additional treatments may be necessary if the aneurysm does not fully close off or if new aneurysms develop over time.
