Loop diuretics are a class of diuretic medications primarily used to treat conditions associated with fluid overload, such as heart failure, chronic kidney disease, and hypertension.
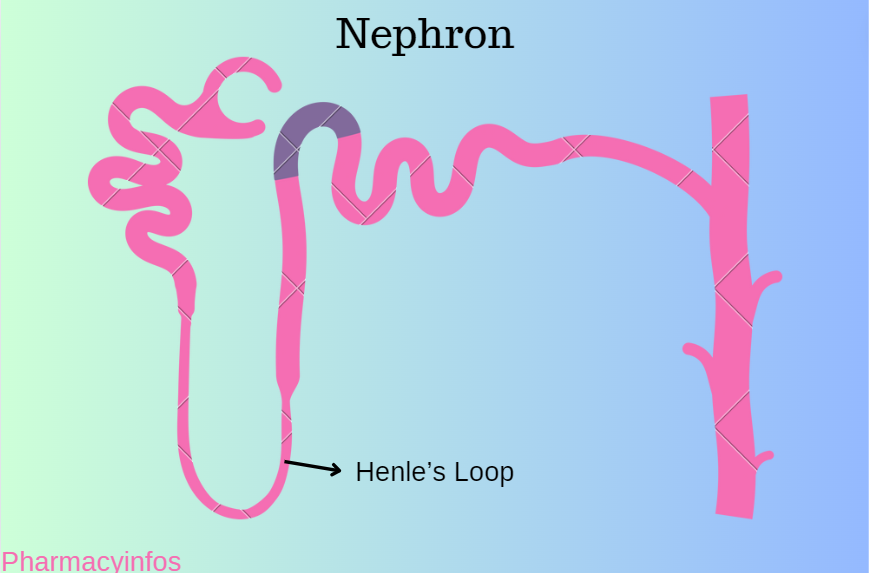
They are among the most potent diuretics available and act on the ascending limb of the loop of Henle in the nephron, a key segment of the renal tubular system.
First we see about the process of diuresis:
Diuresis is the process by which the body increases the production and excretion of urine. This physiological response is essential for maintaining the body’s fluid balance, electrolyte levels, and blood pressure. Diuresis can be influenced by various factors, including hydration status, diet, medications, and underlying medical conditions.
Diuresis process in various organs:
Kidneys: The kidneys are the primary organs responsible for the filtration of blood and the production of urine. They regulate fluid and electrolyte balance by filtering out excess water, salts, and waste products from the bloodstream.
Nephrons: Nephrons are the kidney’s functioning units, and each kidney has about a million of them. Each nephron is made up of a tubule and a glomerulus (a network of capillaries). The glomerulus filters blood, and the tubule reabsorbs needed substances back into the blood while excreting waste products into the urine.
Hormonal Regulation: Several hormones play a crucial role in regulating diuresis:
Antidiuretic Hormone (ADH): Produced by the hypothalamus and released by the posterior pituitary gland, ADH increases water reabsorption in the kidneys, reducing urine output.
Aldosterone: Secreted by the adrenal glands, aldosterone promotes sodium reabsorption in the kidneys, which in turn promotes water retention and reduces urine volume.
Atrial Natriuretic Peptide (ANP): Released by the heart’s atria in response to increased blood volume, ANP promotes sodium and water excretion, increasing urine output.
Osmotic Gradient: The concentration gradient in the renal medulla allows for the reabsorption of water and solutes. The loop of Henle in the nephron creates this gradient, facilitating the concentration or dilution of urine depending on the body’s needs.
Types of Diuresis
Osmotic Diuresis: Occurs when substances such as glucose or mannitol enter the kidney tubules and create an osmotic pressure that pulls water into the urine. This is commonly seen in uncontrolled diabetes mellitus.
Water Diuresis: Happens when excess water is ingested, diluting the blood and decreasing the secretion of ADH. This leads to increased urine output to expel the surplus water.
Pharmacological Diuresis: Induced by diuretic medications, which are used to treat conditions like hypertension, heart failure, and edema. Different classes of diuretics work through various mechanisms to increase urine output,
such as:
- Loop diuretics: Prevent sodium from being reabsorbed in the Henle loop.
- Thiazide Diuretics: Inhibit sodium reabsorption in the distal convoluted tubule.
- Potassium-Sparing Diuretics: Inhibit sodium reabsorption in the collecting ducts while conserving potassium.
Mechanism Of Action:
Loop diuretics inhibit the sodium-potassium-chloride (Na⁺-K⁺-2Cl⁻) cotransporter in the thick ascending limb of the loop of Henle. This transporter normally reabsorbs approximately 25-30% of the filtered sodium load. By inhibiting this cotransporter, loop diuretics prevent sodium and chloride reabsorption, leading to:
Increased Sodium and Chloride Excretion: The inhibition of sodium and chloride reabsorption results in their increased excretion in the urine.
Water Excretion: Due to the osmotic gradient, water follows the excreted sodium and chloride, increasing urine output.
Decreased Reabsorption of Calcium and Magnesium: Loop diuretics also reduce the reabsorption of calcium and magnesium, leading to their increased excretion.
Potassium Excretion: The increased flow of sodium to the distal parts of the nephron promotes potassium secretion and excretion, which can lead to hypokalemia.
Pharmacokinetics:
Loop diuretics are typically administered orally or intravenously, and their effects are rapid. Commonly used loop diuretics include:
Furosemide (Lasix): Often used for acute and chronic conditions requiring potent diuresis.
Bumetanide (Bumex): Similar to furosemide but more potent on a milligram-to-milligram basis.
Torsemide (Demadex): Has a longer duration of action and may be more effective in patients with chronic kidney disease.
Ethacrynic Acid (Edecrin): Used primarily in patients allergic to sulfonamide-derived diuretics, although it has a higher risk of ototoxicity.
Uses of loop diuretics:
1. Heart Failure:
Loop diuretics are crucial in managing both acute and chronic heart failure:
Acute Heart Failure: Loop diuretics are used to rapidly reduce fluid overload and relieve symptoms such as pulmonary edema and shortness of breath. They improve cardiac output and reduce the workload on the heart.
Chronic Heart Failure: They help maintain fluid balance, preventing the recurrence of edema and improving the patient’s quality of life.
2. Edema:
Edema, or swelling due to fluid retention, can result from various conditions, and loop diuretics are effective in treating:
Pulmonary Edema: By reducing fluid in the lungs, loop diuretics improve respiratory function.
Peripheral Edema: Loop diuretics help alleviate swelling in the extremities caused by conditions like heart failure, liver cirrhosis, and nephrotic syndrome.
Liver Cirrhosis: They manage ascites (fluid accumulation in the abdomen) and peripheral edema by reducing the body’s overall fluid burden.
Nephrotic Syndrome: Loop diuretics help manage fluid retention in patients with kidney disease where the kidneys fail to excrete excess fluid.
3. Hypertension:
While not typically first-line treatment for hypertension, loop diuretics are useful in certain situations:
Resistant Hypertension: In patients who do not respond adequately to other antihypertensive medications, loop diuretics can be added to achieve better blood pressure control.
Chronic Kidney Disease: They are particularly effective in managing hypertension in patients with reduced kidney function.
4. Chronic Kidney Disease (CKD):
Loop diuretics are effective in managing fluid overload and hypertension in patients with CKD:
Fluid Overload: They help remove excess fluid, thereby reducing the risk of complications like heart failure and hypertension.
Improving Renal Function: By reducing fluid volume and pressure, they can help preserve remaining kidney function.
5. Acute Kidney Injury (AKI):
Loop diuretics can be used in specific cases of AKI:
Volume Management: In patients with fluid overload, they help manage volume status and improve urine output, though their role in AKI management is more limited and often debated.
6. Hypercalcemia:
Loop diuretics, especially furosemide, are used to treat hypercalcemia (high calcium levels in the blood):
Increased Calcium Excretion: By promoting calcium excretion through the kidneys, loop diuretics help lower blood calcium levels, often in conjunction with intravenous saline to ensure adequate hydration.
7. Hyperkalemia:
In cases of hyperkalemia (high potassium levels in the blood), loop diuretics can help:
Potassium Excretion: By increasing the flow of sodium to the distal nephron, they promote potassium excretion, lowering serum potassium levels.
8. Drug Overdose and Poisoning:
Loop diuretics can be part of forced diuresis protocols to enhance the elimination of certain drugs or toxins from the body:
Rapid Excretion: By increasing urine output, they help flush out toxic substances more quickly, though this approach must be used cautiously under medical supervision.
9. Hypervolemia:
Conditions involving excessive blood volume, such as certain endocrine disorders, can be managed with loop diuretics:
Volume Reduction: They help reduce blood volume, alleviating symptoms and preventing complications associated with hypervolemia.
Clinical Considerations and Monitoring:
While loop diuretics are effective, their use must be carefully monitored to avoid potential adverse effects:
Electrolyte Imbalances: Hypokalemia (low potassium), hyponatremia (low sodium), hypocalcemia (low calcium), and hypomagnesemia (low magnesium) can occur and must be monitored and managed.
Dehydration: Excessive diuresis can lead to dehydration and hypotension.
Renal Function: Regular monitoring of kidney function is essential, especially in patients with preexisting renal impairment.
Hearing Loss: High doses or rapid intravenous administration can cause ototoxicity, leading to hearing loss.
Metabolic Alkalosis: Resulting from excessive loss of chloride and retention of bicarbonate.
Who cannot take the loop diuretics?
People with Severe Hypovolemia or Dehydration: Loop diuretics can exacerbate these conditions by increasing urine output, which can lead to severe fluid loss and electrolyte imbalances.
Patients with Electrolyte Imbalances: Individuals with low levels of potassium (hypokalemia), magnesium (hypomagnesemia), or sodium (hyponatremia) should be cautious. Loop diuretics can worsen these imbalances, leading to serious complications such as arrhythmias.
Individuals with Severe Renal Impairment: While loop diuretics are often used in patients with kidney issues, those with severe renal impairment or anuria (inability to produce urine) may not respond well to these drugs. They can also increase the risk of further renal damage.
Patients with Hypersensitivity to Sulfonamides: Some loop diuretics, like furosemide, contain a sulfonamide group, and patients with sulfonamide allergies may react to these medications.
Pregnant or Breastfeeding Women: Loop diuretics can cross the placenta and are excreted in breast milk, potentially causing harm to the fetus or infant. They are generally avoided unless absolutely necessary and prescribed by a healthcare provider.
Individuals with Gout: Loop diuretics can increase uric acid levels, potentially triggering gout attacks. Patients with a history of gout should be cautious.
Patients on Ototoxic Medications: Loop diuretics have the potential to cause ototoxicity (damage to the ears), especially when taken with other ototoxic drugs like aminoglycoside antibiotics.
It is crucial for anyone considering or prescribed loop diuretics to consult with their healthcare provider to ensure the medication is appropriate for their specific health condition and to discuss any potential risks or contraindications.
