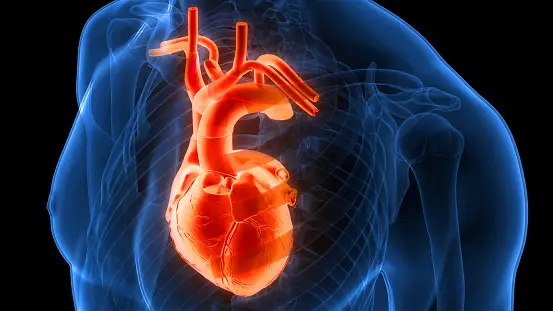
Amlodipine is a drug that is mostly used to treat angina (chest discomfort) and hypertension (high blood pressure). It is a part of the calcium channel blocker (CCB) drug class. Amlodipine works by relaxing and widening the blood vessels, allowing blood to flow more easily and lowering blood pressure. It also increases the supply of blood and oxygen to the heart muscle, which can help reduce the frequency and severity of angina attacks.
Mechanism Of Action Of Amlodipine:
Amlodipine is a medication classified as a calcium channel blocker (CCB). Its mechanism of action involves blocking the influx of calcium ions into smooth muscle cells lining arteries and cardiac muscle cells. By doing so, amlodipine inhibits the contractile process of these muscles, leading to vasodilation (widening of blood vessels) and decreased peripheral vascular resistance.
This mechanism helps to reduce blood pressure and relieve symptoms of angina by increasing blood flow and oxygen supply to the heart muscle.
Bioavailability:
The bioavailability of a medication refers to the proportion of the administered dose that reaches systemic circulation unchanged and is available to exert its therapeutic effects.
For amlodipine, its bioavailability after oral administration is relatively high, typically around 60-65%. However, it can vary among individuals due to factors such as metabolism, absorption, and other physiological differences.
Food can affect the bioavailability of amlodipine. Taking the medication with a meal can slightly decrease its absorption rate, but the overall extent of absorption remains relatively unchanged. Therefore, amlodipine can be taken with or without food, according to healthcare provider instructions.
It’s important to note that while bioavailability provides insight into how much of a drug is absorbed into the bloodstream, it doesn’t necessarily indicate the drug’s efficacy or potency. Other factors such as distribution, metabolism, and elimination also play crucial roles in determining the drug’s overall effectiveness.
Amlodipine Uses:
Hypertension (High Blood Pressure): Amlodipine is commonly prescribed to lower high blood pressure. It functions by letting blood flow more freely, relaxing blood vessels, and minimizing the stress on the heart. By effectively lowering blood pressure, amlodipine helps reduce the risk of heart attacks, strokes, and other cardiovascular complications associated with hypertension.
Angina (Chest Pain): It is also used to treat chronic stable angina, a type of chest pain caused by reduced blood flow to the heart muscle. By dilating the coronary arteries and increasing blood flow to the heart, amlodipine helps relieve angina symptoms such as chest pain or discomfort. It can be used alone or in combination with other medications for angina management.
Amlodipine Overdose:
Severe Hypotension (Low Blood Pressure): Excessive vasodilation caused by amlodipine overdose can lead to a significant drop in blood pressure, resulting in symptoms such as dizziness, lightheadedness, fainting, and weakness.
Tachycardia (Rapid Heart Rate): In response to low blood pressure, the heart may beat faster to compensate, leading to palpitations, rapid heartbeat, or even arrhythmias (irregular heart rhythms).
Peripheral Vasodilation: Amlodipine overdose can cause excessive dilation of peripheral blood vessels, resulting in flushing, warmth, or swelling of the extremities.
Shock: In severe cases, particularly if not promptly treated, amlodipine overdose can lead to a state of shock, characterized by extreme hypotension and inadequate tissue perfusion.
Gastrointestinal Symptoms: Nausea, vomiting, and abdominal pain may also occur as a result of amlodipine overdose.
Precautions:
Hypotension (Low Blood Pressure): Amlodipine can cause a decrease in blood pressure, particularly when initiating therapy or increasing the dosage. Caution should be exercised, especially in patients with pre-existing hypotension or conditions predisposing them to hypotension, such as dehydration, heart failure, or volume depletion.
Liver Function Impairment: Amlodipine is primarily metabolized by the liver. Patients with hepatic impairment may experience increased drug levels and prolonged effects. Dosage adjustments may be necessary in these individuals, and close monitoring of liver function is recommended.
Heart Failure: While amlodipine is generally considered safe for use in patients with heart failure, caution should be exercised, especially in those with severe heart failure or compromised cardiac function. Amlodipine’s vasodilatory effects can exacerbate heart failure symptoms in some cases.
Aortic Stenosis: Amlodipine should be used with caution in patients with severe aortic stenosis (narrowing of the main valve of the heart). Vasodilators like amlodipine may increase the risk of heart failure or myocardial infarction in these individuals.
Elderly Patients: Elderly patients may be more sensitive to the effects of amlodipine, particularly regarding hypotension. Lower initial doses may be considered, and close monitoring for adverse effects is important.
Pregnancy and Breastfeeding: Amlodipine is classified as a Pregnancy Category C medication, meaning its safety in pregnancy has not been well established. It should only be taken if the possible advantages balance the possible hazards to the developing fetus during pregnancy. Amlodipine is excreted in breast milk, so caution should be exercised when breastfeeding.
Pediatric Use: The safety and effectiveness of amlodipine in pediatric patients have not been established. It is generally not recommended for use in children under 6 years of age, and caution should be exercised in older pediatric populations.
Amlodipine Drug Interactions:
Antihypertensive Medications: Combining amlodipine with other antihypertensive drugs, such as beta-blockers, ACE inhibitors, or diuretics, may result in additive blood pressure-lowering effects. However, careful monitoring is necessary to avoid excessive hypotension.
CYP3A4 Inhibitors: Amlodipine is primarily metabolized by the liver enzyme CYP3A4. Drugs that inhibit CYP3A4 activity, such as certain antibiotics (e.g., clarithromycin, erythromycin), antifungal agents (e.g., ketoconazole, itraconazole), and protease inhibitors (e.g., ritonavir), can increase amlodipine levels in the body, increasing the possibility of adverse effects.
CYP3A4 Inducers: Conversely, drugs that induce CYP3A4 activity, such as rifampin, carbamazepine, and St. John’s wort, may decrease amlodipine levels, potentially reducing its effectiveness.
Grapefruit Juice: Grapefruit juice contains compounds that can inhibit CYP3A4 enzymes, leading to increased amlodipine levels. Consuming grapefruit juice while taking amlodipine may potentiate its effects and increase the risk of adverse reactions.
Cyclosporine and Tacrolimus: These immunosuppressant drugs can increase amlodipine levels, potentially leading to toxicity. Close monitoring of blood pressure and amlodipine-related side effects is necessary when co-administering these medications.
Simvastatin: Amlodipine can increase the blood levels of simvastatin, a cholesterol-lowering medication, potentially increasing the risk of muscle-related side effects such as myopathy or rhabdomyolysis. Lower doses of simvastatin may be necessary when used concomitantly with amlodipine.
Other Cardiovascular Medications: Certain medications used to treat cardiovascular conditions, such as diltiazem, verapamil, and quinidine, may interact with amlodipine, potentially causing additive effects on heart rate and blood pressure.
Potassium-Sparing Diuretics: Concurrent use of amlodipine with potassium-sparing diuretics (e.g., spironolactone, triamterene) may increase the risk of hyperkalemia (elevated blood potassium levels). Close monitoring of potassium levels is advisable in such cases.
Side Effects:
Common side effects of amlodipine may include dizziness, headache, fatigue, flushing, peripheral edema (swelling of the ankles or feet), and palpitations. These adverse effects are usually mild and transient. However, serious side effects such as severe hypotension (low blood pressure), heart rhythm disturbances, and allergic reactions are possible but rare.
